Special Report: ADHD Treatments Scorecard from ADDitude Readers
An exclusive survey of 11,000 ADDitude readers reveals the treatment approaches they recommend most, common side effects, and barriers to quality care.
ADHD medication remains a magnet for debate, confusion, and promise.
Amphetamine and methylphenidate have been used to treat ADHD for at least 80 years, and their safety and efficacy have been studied relentlessly. But according to a recent ADDitude survey, less than half (42%) of parents opt to medicate their children in the months after a diagnosis, largely due to the fear of real or perceived side effects like appetite suppression or sleep disruption — both possible impediments to growth.
In the end, 85% of all people with ADHD end up taking medication and they rate its efficacy higher than any other treatment approach included in the survey, ADDitude’s largest to date. More than 11,000 adults with ADHD and caregivers of children with the condition participated in the survey from July to December 2023.
“We hesitated for a long time and tried diet changes first in an attempt to avoid medication,” said one respondent. “Although diet is very important, medication has given our child the opportunity to enjoy life by having more emotional control, better friendships, and the ability to complete work and think things through. Greater self-confidence flows from all of this.”
Most Popular ADHD Medications
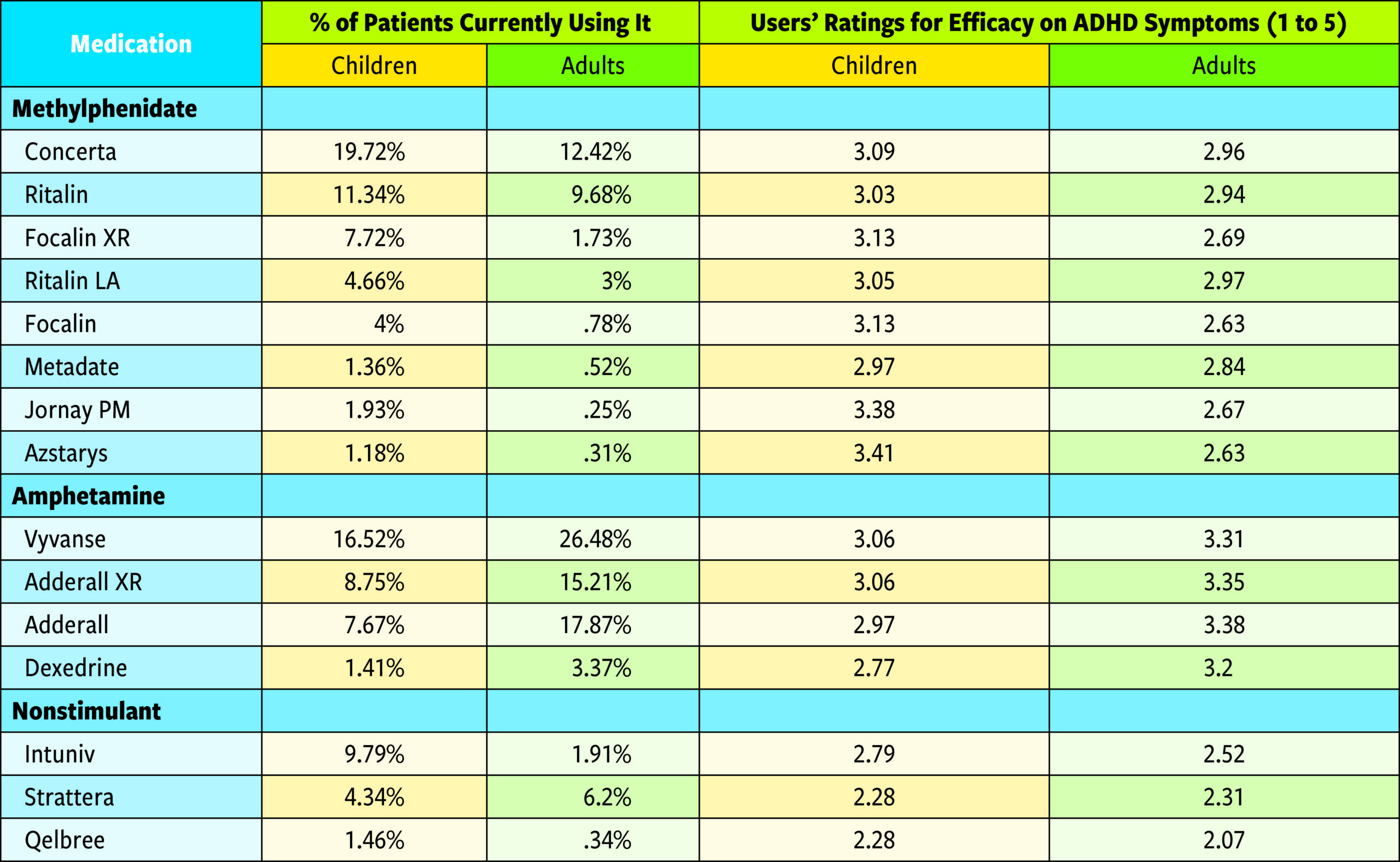
To be clear, ADHD medication is not a quick fix. On average, children try 2.75 different medications and adults try 2.56 prescriptions before finding one that works for them. Survey respondents also said that 17% of children and 14% of adults cease treatment with medication for one reason or another — cessation rates lower than reported in other studies.1
Biggest Impediments to ADHD Treatment
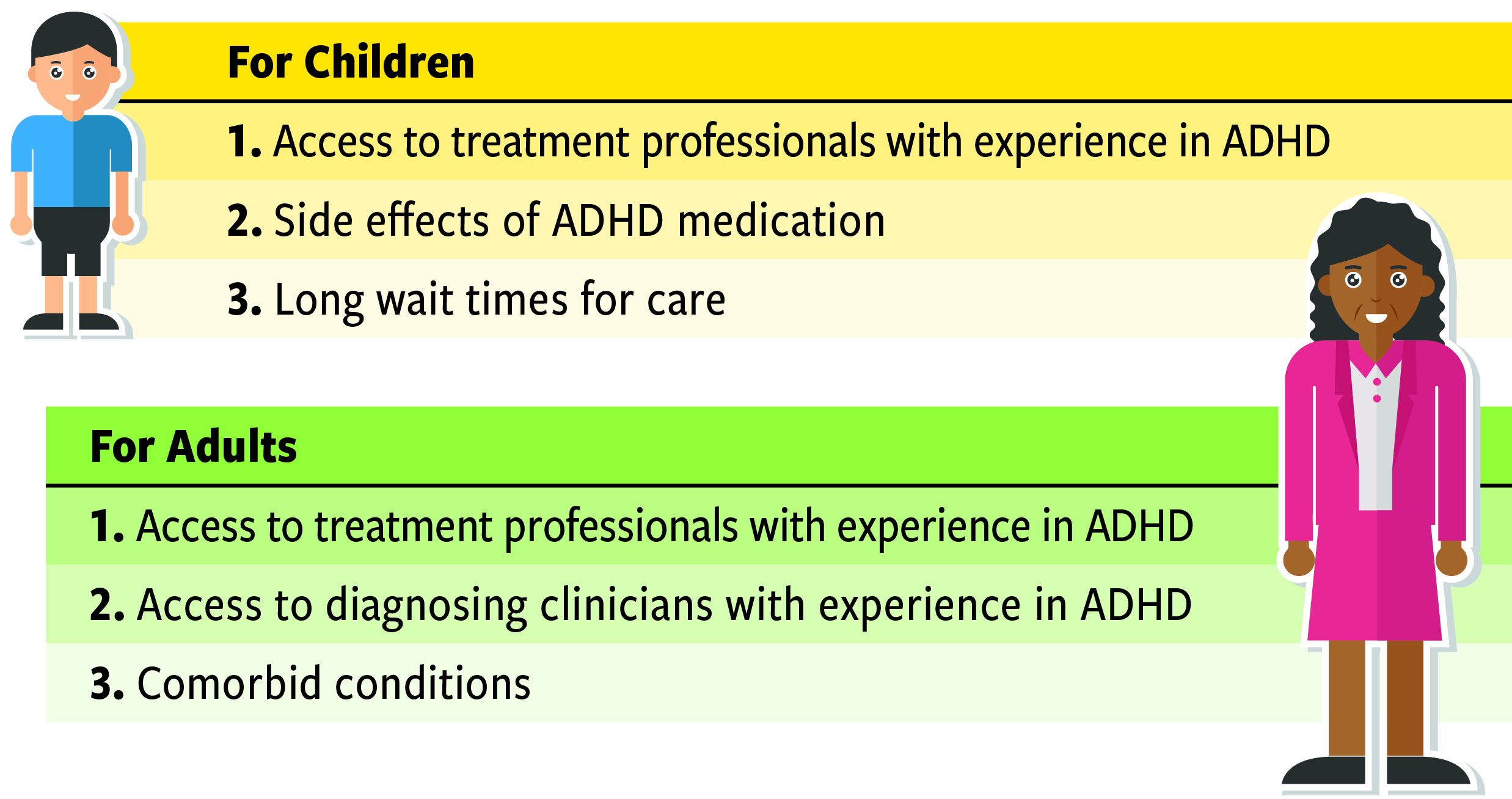
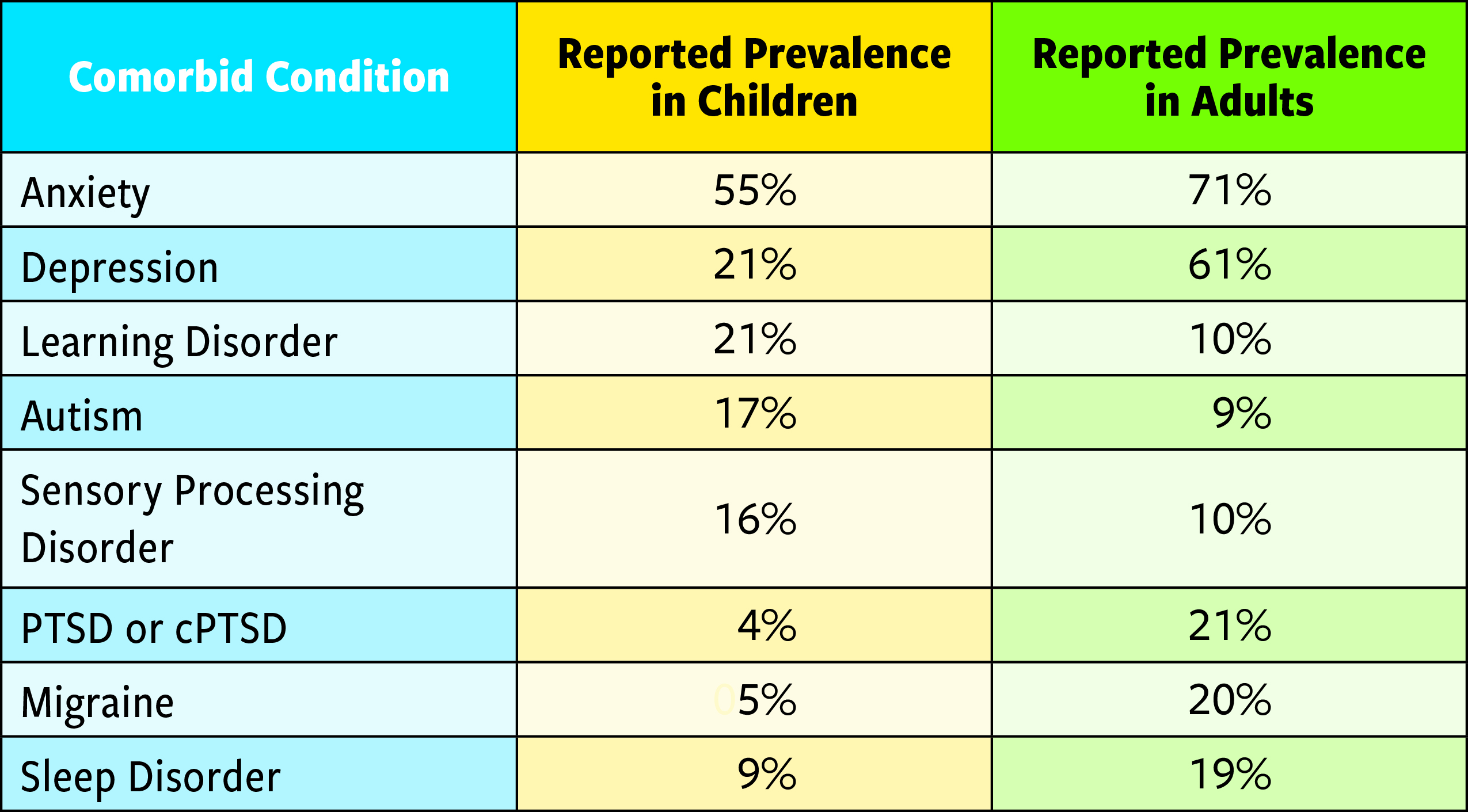
Access to treatment professionals with experience in ADHD is the biggest impediment to effective treatment, according to both caregivers and adults. Other barriers include side effects, long wait times, poor access to diagnosing clinicians, and comorbid conditions that complicate evaluation and treatment (82% of children and 92% of adults with ADHD report comorbid diagnoses).
ADHD’s Most Common Comorbid Conditions
The average age of ADHD diagnosis in children is 8 for boys and 9 for girls, according to survey respondents. On average, adults not diagnosed as children learn of their ADHD around age 39. Most of these late diagnoses are among women, who report years of struggle preceding their diagnosis.
“I wish I had been diagnosed and treated sooner,” wrote one survey respondent. “The struggle is so profound and deep. And the longer you go through it without help or knowing what you’re really struggling with, the harder it feels to get others to hear and see you. You feel alone.”
Persistence, flexibility, and self-advocacy are vitally important when working to find the right medication. Though the trial-and-error phase was described as frustrating by most survey respondents, research tells us the benefits of ADHD medication use — reduced risks of automobile accidents, substance abuse, unwanted pregnancy, sexually transmitted diseases, and self harm in teens — are worthwhile and meaningful.2
“I wish I had known that ADHD medication helps prevent addictions to dangerous substances,” wrote one survey respondent, “and car accidents for people with ADHD.”
ADHD Medication Formulation, Duration & Satisfaction
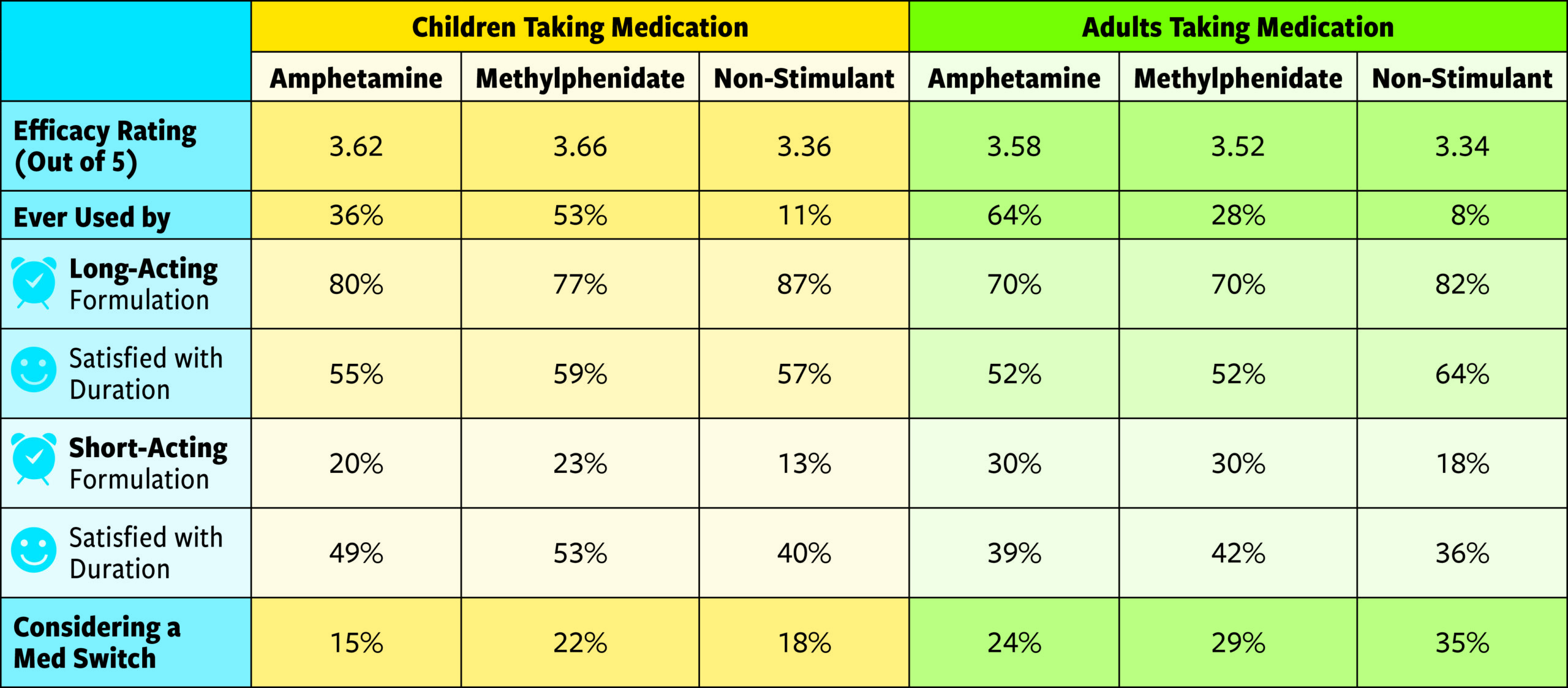
Barely half of patients taking a long-acting medication are satisfied with its duration of coverage, which is 9.5 hours for children and 10 hours for adults, on average. This is a flunking grade, but it’s far superior to the satisfaction ratings for short-acting formulations. So why do up to 23 percent of children and 30 percent of adults take short-acting stimulants? Perhaps because clinicians are more likely to prescribe them, and some adults like the medications’ relative flexibility.
“Sometimes, in a social setting, I quite like taking only 5 mg of short-release (rather than my prescribed 10 mg),” wrote one survey respondent. “Other times, when working on something that I find really dull, I often take 15 mg (3 x 5 mg tablets).”
In the end, adults are more likely than children to take short-acting formulations, to be dissatisfied with their medications, and to be considering a switch, according to the survey data.
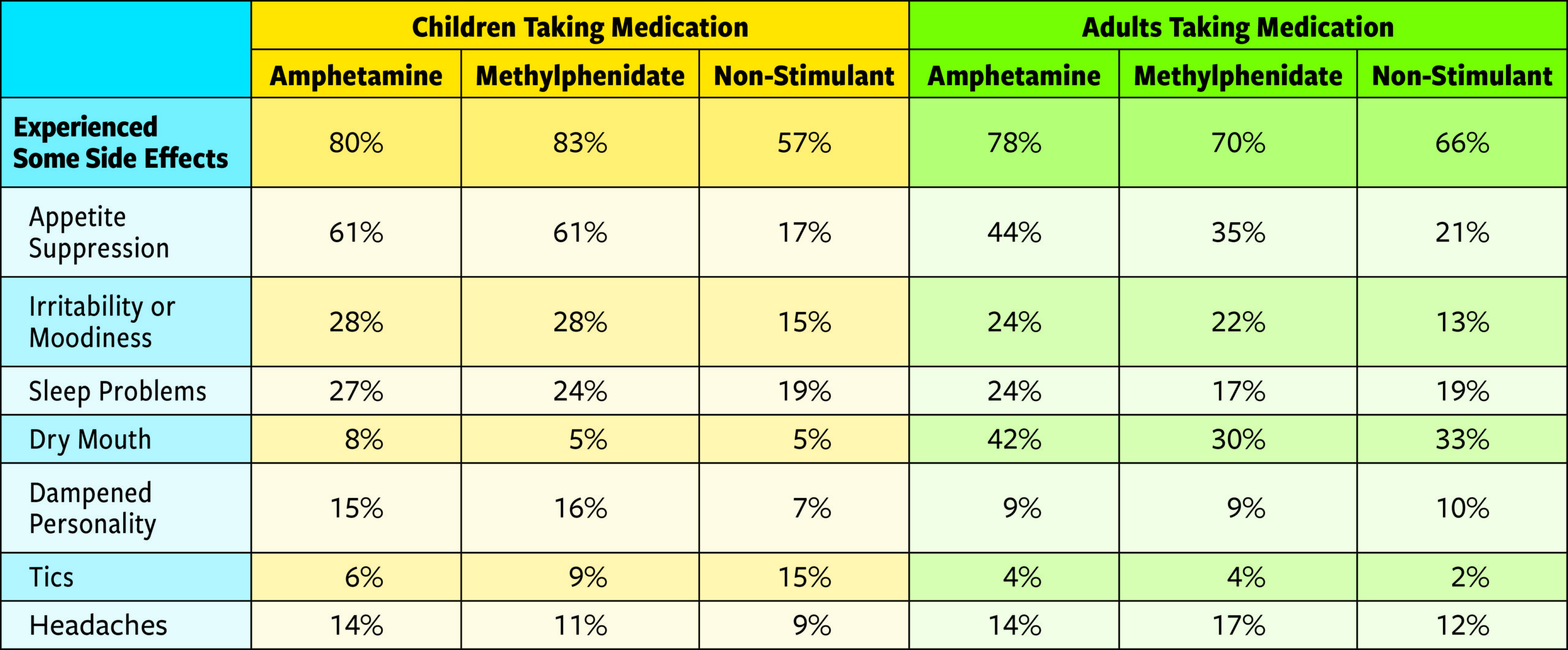
ADHD Medication Side Effects
Caregivers are likely to try fish oil, eliminate food dyes, and sign up for karate before considering a prescription for their child. Once they decide to try medication, caregivers prioritize finding the one with the fewest side effects.
At the same time, 53% of children who end up taking medication try methylphenidate, 36% take amphetamine, and just 11% take a non-stimulant. So given its popularity, methylphenidate must deliver the fewest side effects, right?
No. According to caregiver reports, slightly more children reported side effects from methylphenidate than amphetamine, and those side effects were nearly identical, with appetite suppression being the most common by far; it impacted 61% of children taking any stimulant.
Adults use amphetamine for what they cite as their top priority in choosing a medication: symptom control. Yet they gave it an efficacy rating that was only slightly better than methylphenidate, which is associated with fewer side effects.
So should more adults consider trying Concerta, Ritalin, or a newcomer like Azstarys? One-quarter to one-third of adults said they are now considering some kind of medication switch.
ADHD Treatments Scorecard
Most Highly Recommended ADHD Treatment Approaches
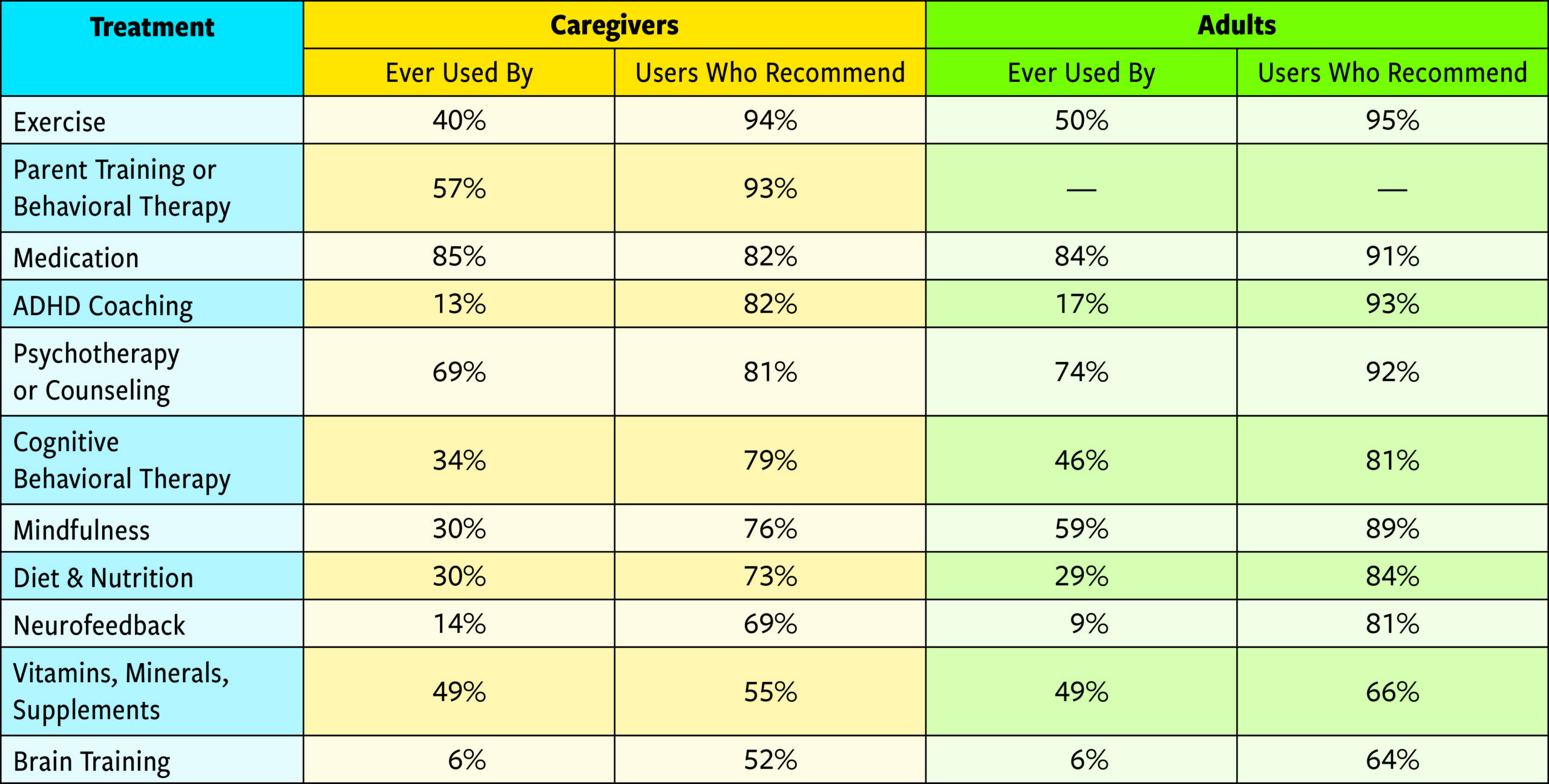
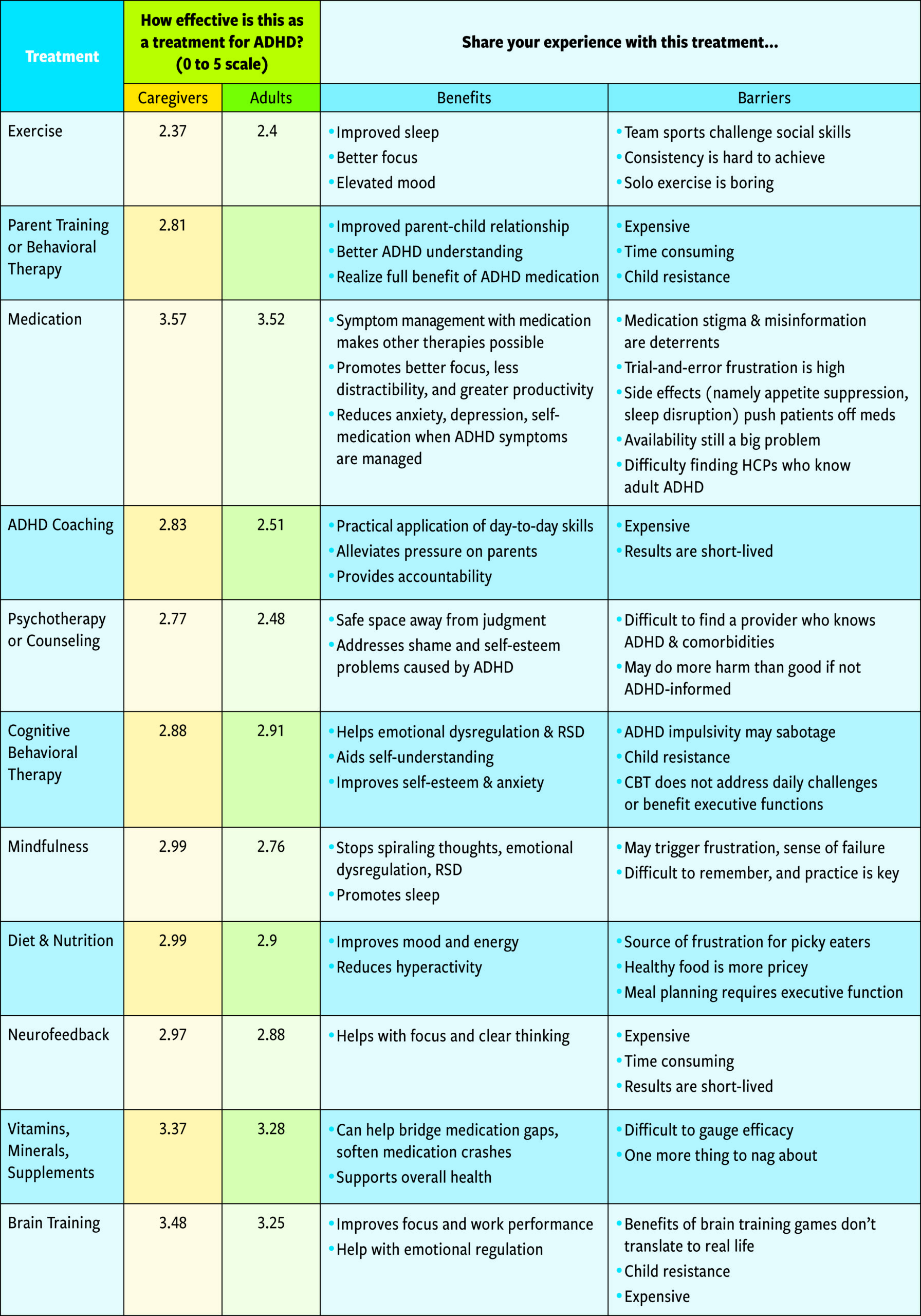
ADHD Treatment Approaches with Highest Efficacy Ratings
Rated According to Effectiveness on ADHD Symptoms, Specifically
What Readers Say vs. What They Do
The most highly recommended approach to managing ADHD symptoms (exercise) has been used by less than half of ADDitude survey respondents. The second most recommended approach among adults (ADHD coaching) has been adopted by only 17 percent of people. And the vitamins, minerals, and supplements used by 49 percent of people surveyed don’t even earn a passing grade. All of this hints at problems with availability, cost, and medical advice in the world of ADHD treatment.
Diet and Nutrition Approaches for ADHD
What dietary changes move the needle?
At least half of caregivers and adults reported that the following dietary changes have a positive impact on ADHD symptoms:
- Decreasing or eliminating artificial colors/preservatives/sweeteners3
- Decreasing or eliminating sugar4
- Increasing protein
Research generally supports these observations and reader efficacy ratings are high. So why are fewer than 30% of caregivers and adults making dietary changes to address ADHD? For one, 61% of children using stimulant medication to treat their ADHD experience appetite suppression as a side effect, according to their caregivers. Dietitians generally advise that children should focus on eating first and eating heathy second.
“We struggle to get enough calories into our child due to decreased appetite,” wrote one parent. “We are happy to have her eat, regardless of what or when, to keep energy levels up.”
Psychotherapy More Prevalent Than ADHD Coaching
Though the recommendation rates are nearly identical, far more people engage in psychotherapy than work with an ADHD coach. Therapy generally helps clients work through comorbid conditions like anxiety and depression, and negative beliefs or self-defeating behaviors. Coaching helps to strengthen skills to mitigate ADHD deficits and reach goals, but its benefits are short-lived, readers say.
“ADHD coaching helped me to narrow down my biggest challenges and work on practical solutions for the day-to-day things I struggle with,” said one survey respondent.
Parent Training or Behavioral Therapy for ADHD
This first-line treatment is used by less than 6 out of 10 study participants.
The American Academy of Pediatrics recommends parent training in behavior management as a first-line ADHD treatment for children diagnosed before age 7, and a complementary treatment approach thereafter. Despite this recommendation, and a high rate of reported satisfaction, just more than half of parents say they’ve ever used it. Possible reasons for this: Clinicians aren’t recommending parent training nearly enough; behavioral therapists versed in ADHD are difficult to find; and/or therapy is expensive and time-consuming. Likely, all of these reasons are true.
“Changing the way we parented was a game changer,” wrote one survey respondent. “It brought the stress in the house down significantly and meant we could focus on the lagging skills and promoting the behaviors we wanted to see versus punishing behaviors we didn’t want to see.”
Exercise Is Invaluable and Infrequent
Does exercise eradicate ADHD symptoms? Hardly. Readers rated its efficacy on ADHD just 2.4 out of 5, but they also called it invaluable — especially vigorous cardiovascular morning exercise. It aids sleep, mood, and hyperactivity, our readers say. So why isn’t exercise a universal component of treatment plans? As we know, the ADHD brain is easily bored and resists routine.
“When I get into a good stride with routine exercise, it almost always goes hand-in-hand with better eating habits, better focus, energy levels, mental clarity, and stronger relationships and productivity,” said one adult with ADHD. “Exercise is undoubtedly a crucial piece of the (treatment) puzzle.”
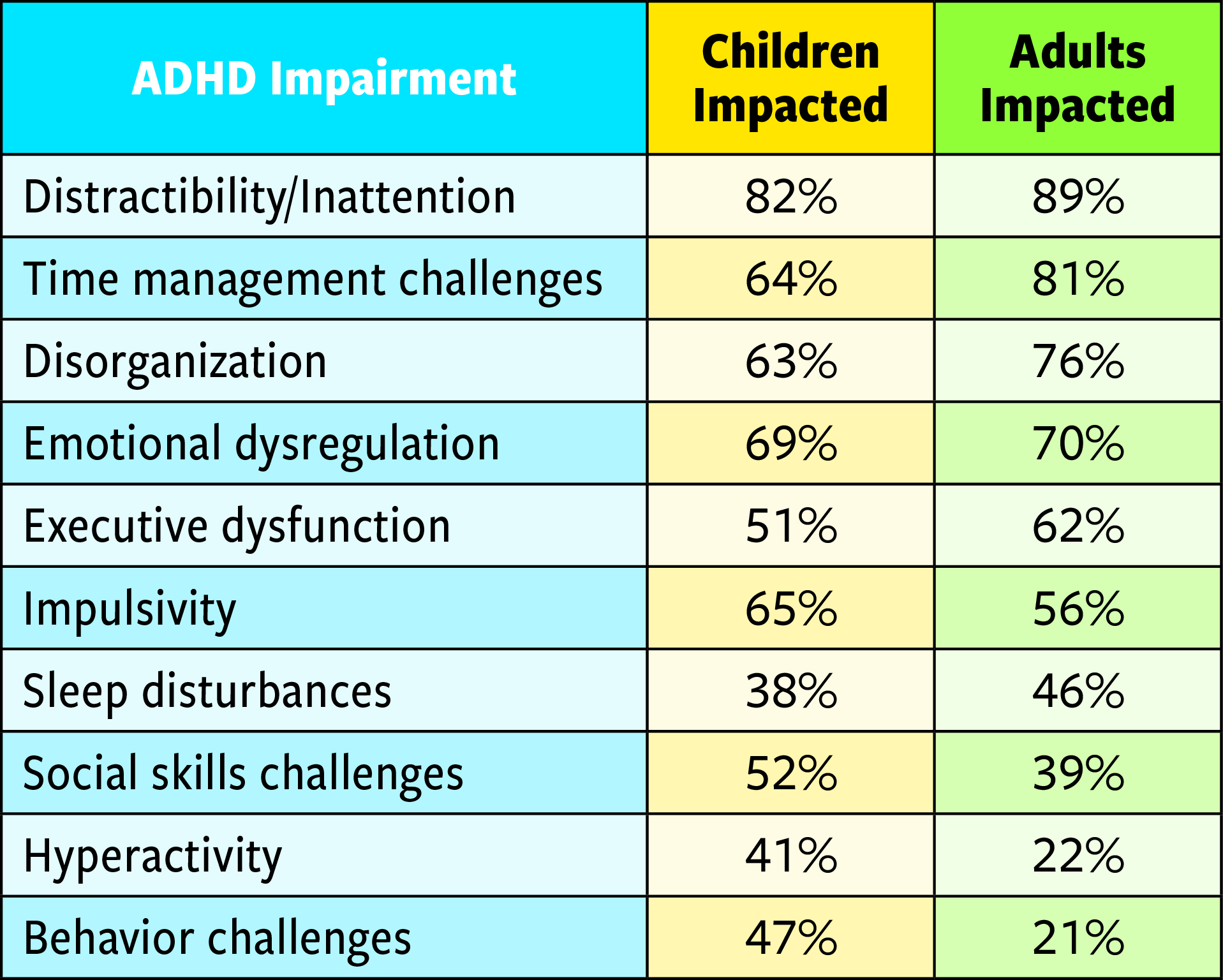
Most Impairing Symptoms of ADHD
ADHD Treatment Options: Next Steps
- Download: Share This Report with Your Doctor
- Read: ADHD Medication Reviews
- Get: The ADHD Treatment Guide for Adults
View Article Sources
1 Brikell I, Yao H, Li L, Astrup A, Gao L, Gillies MB, Xie T, Zhang-James Y, Dalsgaard S, Engeland A, Faraone SV, Haavik J, Hartman C, Ip P, Jakobsdóttir Smári U, Larsson H, Man KK, de Oliveira Costa J, Pearson SA, Hostrup Nielsen NP, Snieder H, Wimberley T, Wong IC, Zhang L, Zoega H, Klungsøyr K, Chang Z. ADHD medication discontinuation and persistence across the lifespan: a retrospective observational study using population-based databases. Lancet Psychiatry. 2024 Jan;11(1):16-26. doi: 10.1016/S2215-0366(23)00332-2. Epub 2023 Nov 27. PMID: 38035876.
2 Chang Z, Ghirardi L, Quinn PD, Asherson P, D’Onofrio BM, Larsson H. Risks and Benefits of Attention-Deficit/Hyperactivity Disorder Medication on Behavioral and Neuropsychiatric Outcomes: A Qualitative Review of Pharmacoepidemiology Studies Using Linked Prescription Databases. Biol Psychiatry. 2019 Sep 1;86(5):335-343. doi: 10.1016/j.biopsych.2019.04.009. Epub 2019 Apr 17. PMID: 31155139; PMCID: PMC6697582.
3 Rambler RM, Rinehart E, Boehmler W, Gait P, Moore J, Schlenker M, Kashyap R. A Review of the Association of Blue Food Coloring With Attention Deficit Hyperactivity Disorder Symptoms in Children. Cureus. 2022 Sep 16;14(9):e29241. doi: 10.7759/cureus.29241. PMID: 36262950; PMCID: PMC9573786.
4 Johnson RJ, Wilson WL, Bland ST, Lanaspa MA. Fructose and uric acid as drivers of a hyperactive foraging response: A clue to behavioral disorders associated with impulsivity or mania? Evol Hum Behav. 2021;42(3):194-203. doi:10.1016/j.evolhumbehav.2020.09.006






